5 Myths About Using Suboxone to Treat Opioid Addiction What Is Suboxone and Why Does It Matter?
For years now, the fight against opioid addiction in the United States has been an uphill climb, one that has claimed far too many lives. Amid the noise, fear, and misinformation, a quiet hero has emerged: Suboxone.
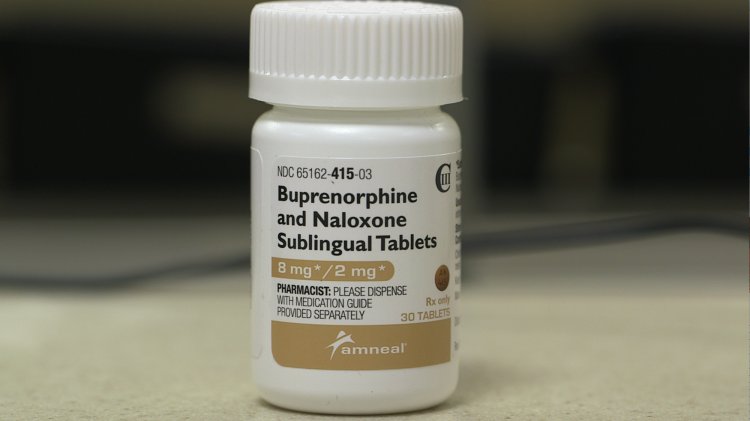
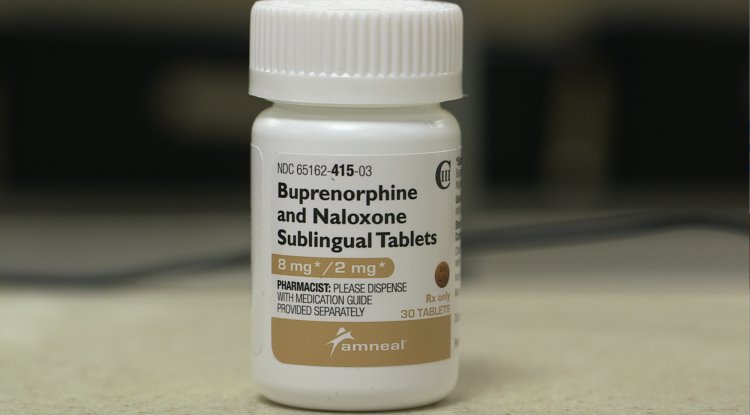
Suboxone is a combination of two medications buprenorphine and naloxone and it’s changing what recovery looks like for thousands of people. Buprenorphine connects to the same receptors in the brain that opioids do, but in a slower, gentler way. It keeps withdrawal symptoms and cravings in check without causing the dizzying highs that fuel addiction. Naloxone, meanwhile, acts as a safety guard blocking the effects if someone tries to misuse it.
This medication falls under a larger, evidence-based approach known as Medication for Opioid Use Disorder (MOUD). Studies have shown that people on MOUD are 50% less likely to die from an overdose, and far less likely to relapse.
At a time when the United States loses more than 100,000 people each year to opioids, Suboxone isn’t a luxury. It’s a lifeline.
Recently, the government made a crucial change: doctors no longer need a special “X-waiver” to prescribe it.For thousands of people who had been waiting far too long for assistance, that one change in policy opened doors.
Still, even as medical understanding grows, the public conversation often lags behind. Myths and stigma continue to shadow this lifesaving
medication and those myths can stop people from getting care they desperately need.
Let’s take a closer look at five of the most common misconceptions about Suboxone, and what science and real life have to say.
Myth#1: is that "you are not really in recovery if you are using Suboxone."

Reality: Recovery is by no means a contest of purity, nor is there a one-size-fits-all strategy.
This myth comes from older, abstinence-only models of recovery like the ones that shaped mid-century addiction programs such as Alcoholics Anonymous. The belief was simple: if you’re taking anything, even medication prescribed by a doctor, you’re not truly “sober.”
But we’ve learned a lot since then. Addiction isn’t a moral flaw, it's a medical condition. And for many, Suboxone is what allows their brain chemistry to heal and stabilize. It’s what lets them rebuild relationships, return to work, and live without chaos.
To tell someone they aren’t “really” in recovery because they take a prescribed medication is not just inaccurate, it's cruel. Recovery isn’t about abstaining from a pill; it’s about reclaiming control over your life.
Myth #2: "Suboxone abuse occurs frequently."
Reality: Misuse occurs much less frequently than people realize, and when it does, it is typically the result of desperation rather than carelessness.
Other opioids are not like suboxone. It only partially stimulates the opioid receptors in the brain since it is a partial agonist.
. That built-in ceiling effect limits euphoria so while it helps with withdrawal and cravings, it doesn’t create the same high that drugs like heroin or fentanyl do.
In truth, most people who take Suboxone without a prescription aren’t trying to get high. They’re trying to get better to manage withdrawal symptoms, to stay functional, to keep from spiraling. If Suboxone were
easier to access through legitimate medical channels, people wouldn’t feel forced to self-treat in unsafe ways.
So rather than viewing these individuals as offenders, maybe we should see them as people doing their best to survive in a system that hasn’t always met them halfway.
Myth #3: "Taking too much Suboxone is just as easy as taking too much of any other opiate."

The truth is that taking too much Suboxone by itself is nearly impossible.
This is the reason: Buprenorphine has a ceiling effect, which means that consuming more does not increase its effects when you have reached a particular dosage. Suboxone is significantly safer than conventional opioids, which have no upper limit and can cause fatal respiratory slowdowns, thanks to this built-in safety feature.
The majority of overdoses caused by suboxone occur when users combine it with other drugs, such as alcohol or benzodiazepines. Suboxone by itself is among the safest drugs used to treat addiction nowadays.
It is a safeguard against the most harmful aspects of addiction, not just a medication for recovery.
Myth #4: "You are not receiving effective treatment if you are not in therapy."
Reality: While therapy has its uses, there are other ways to get well.
In an ideal world, everyone struggling with addiction would have access to peer support, therapy, housing, and employment support. Reality, however, is not always cooperative.
The truth is, only one in five people with opioid use disorder in America gets any form of adequate treatment.
That’s why it’s so important to recognize that Suboxone itself is a treatment. Even when therapy isn’t accessible, Suboxone alone dramatically reduces relapse, overdose, and death.
Would recovery outcomes improve with additional support? Absolutely. But denying someone medication until they meet some “ideal” version of recovery only drives them further away from safety.
Healing begins when people are met where they are not where others think they should be.
Myth #5: "Only short-term use of suboxone is recommended."
The truth is that there is no uniform timetable for medication and no timeframe for healing.
Some people use Suboxone for a few months and taper off when they’re ready. Others stay on it for years because it helps them stay stable. There’s no scientific evidence suggesting that short-term treatment works better. In fact, stopping too soon often.
What's Your Reaction?