A New Look at Steroid Injections for Knee and Hip Osteoarthritis
Osteoarthritis is one of the most common and frustrating conditions people face as they age.

The result? Pain, stiffness, and sometimes serious mobility issues.
While age is a big factor, it’s not the whole story. Genetics, body weight, past injuries, and even activity levels all play a role in who develops osteoarthritis. It’s also the leading reason more than a million Americans undergo hip or knee replacements every year.
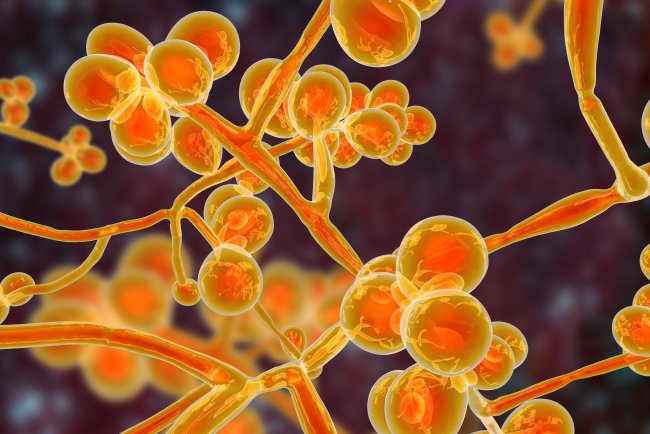
Before surgery, most people try less invasive options: NSAIDs like ibuprofen or naproxen, physical therapy, braces, lifestyle changes like weight loss, and in some cases, injections into the joint itself. Steroid injections in particular have been a popular choice because they can quickly reduce inflammation and ease pain sometimes for weeks or even months.
Steroid injections under the microscope
But new research is raising questions about just how effective and safe these injections really are. A recent review and a medical center’s own findings flagged some concerns:
The overall evidence that steroid injections help isn’t as strong as once believed.
Around 7–8% of patients may actually see their arthritis progress faster than expected after injections.
Rare but serious side effects include unusual fractures (in about 1% of people) and bone damage called osteonecrosis (also about 1%).
More common side effects can include temporary spikes in blood sugar, bleeding in the joint, and occasional infection.
While these numbers are small, they’re enough to give both doctors and patients pause. Some experts now recommend doing x-rays before each injection to screen for early complications, though it’s not clear how much that would help.
So, are steroid injections worth it?
It varies. In actuality, individual experiences differ, even if research may show a tiny average advantage. Some people get only mild, short-term relief, while others feel a significant improvement in pain and mobility for months. For those patients, a carefully limited number of injections usually no more than three or four per year can be life-changing.
Still, there are caveats. If one injection doesn’t help much, it’s usually not worth repeating. And because of the possible risks, injections shouldn’t be treated as a long-term, routine fix.
From here, where do we go?

Steroid injections should not necessarily be eliminated from the therapy arsenal in light of the most recent research. The secret might be to use them more sparingly, limiting the number of injections to a handful per year, giving them to individuals who exhibit noticeable improvement, and carefully balancing the risks and benefits each time.
What’s missing are better studies that tell us who benefits most, and which types or doses of steroids work best with the least downside. Until then, steroid injections remain a “maybe” option helpful for some, less so for others, and best used thoughtfully rather than reflexively.
For patients living with knee or hip osteoarthritis, that means the conversation with your doctor is more important than ever. Relief is possible but the path to it might look different for each person.
What's Your Reaction?